The Importance Of Safe Sexual Practices
When it comes to sexual health, practicing safe sex is of utmost importance. Safe sexual practices not only protect individuals from unwanted pregnancies but also help prevent the spread of sexually transmitted infections (STIs). By being aware of and implementing safe sexual practices, individuals can protect themselves and their partners from potential risks and maintain a healthy sexual life.
One of the key components of safe sexual practices is the use of contraception. Contraception plays a vital role in preventing unintended pregnancies and can be used in various forms, such as condoms, birth control pills, intrauterine devices (IUDs), and more. It is essential for individuals to understand the different types of contraception available and choose the method that best suits their needs and lifestyle. By using contraception consistently and correctly, individuals can reduce the risk of unplanned pregnancies and the potential complications associated with them.
In addition to contraception, communicating with partners about sexual histories, STI testing, and the importance of regular check-ups is crucial. It is essential to have open and honest discussions with sexual partners to ensure mutual consent and prevent the spread of STIs. Consent should always be given and respected during any sexual activity. Seeking consent ensures that both partners are comfortable, willing, and actively participating in sexual encounters.
- Furthermore, education and awareness play a significant role in promoting safe sexual practices. Spreading awareness about the importance of safe sex, contraception methods, and the risks of STIs can empower individuals to make informed decisions regarding their sexual health. Health education programs, both in schools and communities, should prioritize providing accurate and comprehensive information about sexual health. By increasing knowledge and awareness, we can reduce the stigma surrounding sexual health and encourage responsible behavior.
| Benefits of Safe Sexual Practices: |
|---|
| 1. Prevention of unwanted pregnancies: Safe sexual practices such as using contraception significantly reduce the risk of unplanned pregnancies. |
| 2. Protection against STIs: Consistently using barrier methods such as condoms can lower the chances of acquiring or transmitting STIs. |
| 3. Promotes mutual respect and consent: Engaging in open communication and practicing consent ensures that both partners’ boundaries are respected in sexual encounters. |
| 4. Enables a healthy sexual life: By reducing the risk of pregnancy and STIs, safe sexual practices contribute to overall sexual well-being and satisfaction. |
The Role Of Contraception In Pid Prevention
When it comes to preventing pelvic inflammatory disease (PID), there are various factors that come into play. One crucial aspect is the role of contraception in PID prevention. Contraception methods not only help prevent unwanted pregnancies but also protect against sexually transmitted infections (STIs), which can lead to PID. In this blog post, we will explore the different types of contraception and how they contribute to PID prevention.
Barrier methods: These include condoms, both male and female, which act as a physical barrier to prevent the exchange of bodily fluids during sexual intercourse. By using condoms correctly and consistently, individuals can significantly reduce their risk of acquiring STIs, including those that may lead to PID.
Hormonal methods: Hormonal contraception, such as birth control pills, patches, injections, or implants, works by altering the hormonal balance in a person’s body to prevent pregnancy. However, many of these methods also provide protection against STIs. For example, some birth control pills contain a combination of hormones that can help reduce the risk of PID caused by certain STIs.
Intrauterine devices (IUDs): IUDs are small, T-shaped devices that are inserted into the uterus to prevent pregnancy. There are two main types of IUDs: hormonal and non-hormonal. Hormonal IUDs release a progestin hormone, which not only prevents pregnancy but also thickens the cervical mucus, making it difficult for bacteria to enter the uterus and cause infection. Non-hormonal IUDs, often made of copper, work by creating an environment that is toxic to sperm and can also provide some protection against certain STIs and subsequently PID.
- Table:
Contraception Method Advantages Protection Against STIs/ PID Condoms Easy to use, easily accessible Provides a physical barrier against STIs, including those causing PID Birth Control Pills, Patches, etc. Highly effective at preventing pregnancy Some pills offer protection against specific STIs and PID IUDs (Hormonal and Non-hormonal) Long-lasting contraception, minimal maintenance Both types offer protection against certain STIs and PID
Recognizing And Treating Sexually Transmitted Infections (Stis)
Sexually transmitted infections (STIs) are a significant global health issue, affecting millions of individuals each year. They are primarily transmitted through sexual contact, including vaginal, anal, and oral sex. STIs can have serious consequences for individual health, including pelvic inflammatory disease (PID), infertility, and an increased risk of certain types of cancer. Therefore, recognizing and treating STIs is paramount in preventing the spread of these infections and their associated complications.
There are various types of STIs, including chlamydia, gonorrhea, syphilis, genital herpes, human papillomavirus (HPV), and human immunodeficiency virus (HIV). These infections can often have mild or no symptoms, making them difficult to recognize without proper testing. Regular screenings, especially for individuals engaging in high-risk sexual behaviors, are crucial for early detection and prompt treatment.
The first step in recognizing STIs is understanding the common signs and symptoms. For instance, chlamydia and gonorrhea can cause symptoms such as abnormal vaginal or penile discharge, pain during urination, and pelvic pain. Genital herpes often presents as painful blisters or sores in the genital or anal area. Syphilis can manifest as painless sores, rashes, or flu-like symptoms. HPV and HIV may not have visible symptoms in the early stages.
- Chlamydia: Abnormal vaginal or penile discharge, pain during urination, pelvic pain.
- Gonorrhea: Abnormal vaginal or penile discharge, pain during urination, pelvic pain.
- Genital Herpes: Painful blisters or sores in the genital or anal area.
- Syphilis: Painless sores, rashes, or flu-like symptoms.
- HPV: May not have visible symptoms in the early stages.
- HIV: May not have visible symptoms in the early stages.
If you experience any of these symptoms or suspect you may have been exposed to an STI, seeking medical attention promptly is crucial. Early diagnosis and treatment can prevent the spread of infection and reduce the risk of complications. Medical professionals can conduct various tests to diagnose STIs, such as urine tests, blood tests, swabs from genital sores, or pap smears for HPV.
Treatment for STIs typically involves the use of antibiotics or antiviral medications, depending on the specific infection. It is important to complete the full course of treatment as prescribed by a healthcare provider, even if symptoms improve. individuals diagnosed with an STI should inform their sexual partners and encourage them to get tested and treated to prevent reinfection and further spread of the infection.
Preventing the transmission of STIs is equally important. Consistent and correct use of barrier methods, such as condoms, during sexual activity can significantly reduce the risk of infection. It is recommended to have open and honest discussions about sexual health with sexual partners, including previous STI diagnoses and testing history. Regular screenings for STIs, especially for sexually active individuals, can aid in early detection and timely treatment.
Early Detection: Signs And Symptoms Of Pid
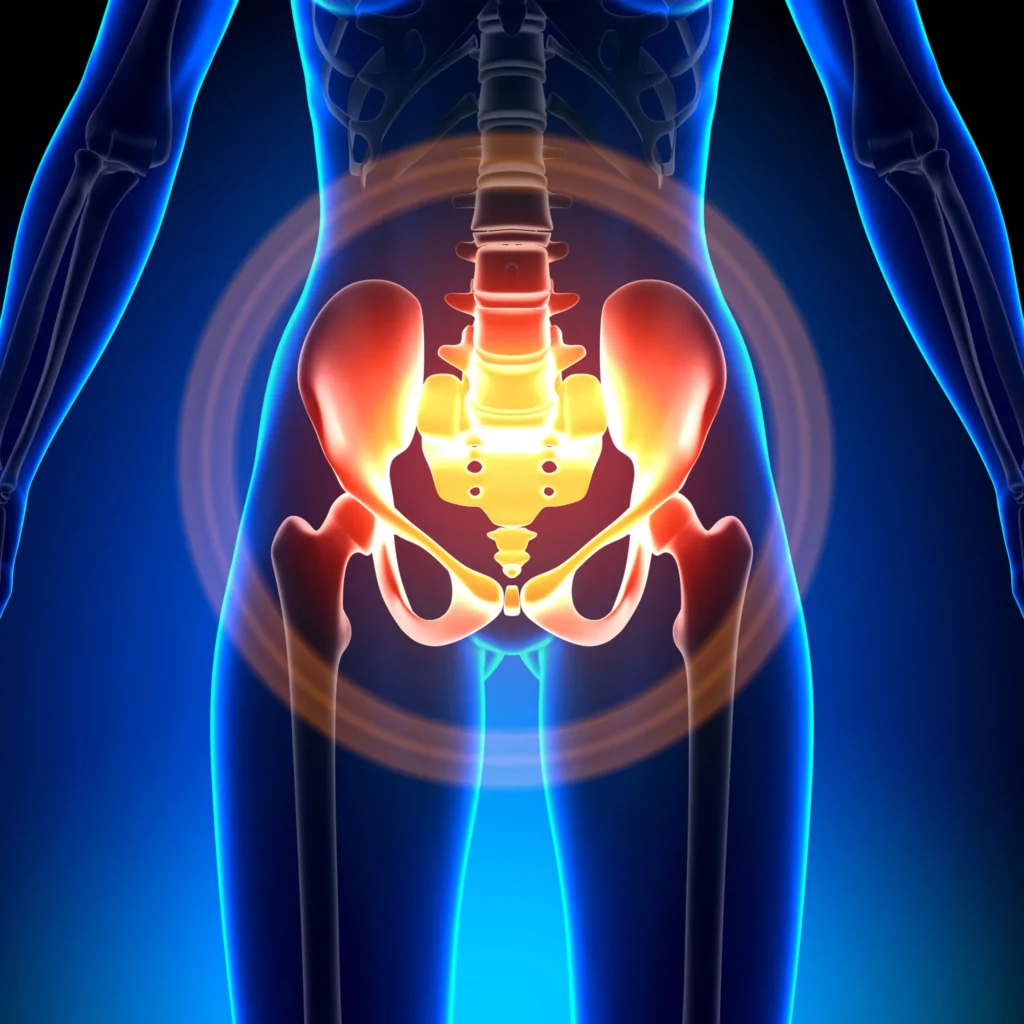
Pelvic Inflammatory Disease (PID) is a serious infection of the female reproductive organs, including the uterus, fallopian tubes, and ovaries. If left untreated, it can lead to severe complications, such as infertility, chronic pelvic pain, and ectopic pregnancy. Early detection of PID is crucial in order to prevent these complications and ensure timely treatment. It is important for women to be aware of the signs and symptoms of PID so that they can seek medical attention as soon as possible.
Common Signs and Symptoms:
1. Lower abdominal pain: One of the most common symptoms of PID is pain or discomfort in the lower abdomen. The pain may range from mild to severe and may be constant or intermittent.
2. Unusual vaginal discharge: Women with PID may experience abnormal vaginal discharge, which may be yellow or green in color, and may have a foul odor.
3. Irregular menstrual bleeding: PID can cause changes in a woman’s menstrual cycle, including irregular bleeding or spotting between periods.
- Other possible signs and symptoms of PID:
- Fever
- Painful urination
- Painful intercourse
- Nausea or vomiting
It is important to note that not all women with PID will experience the same symptoms, and some women may not have any symptoms at all. Therefore, it is crucial for sexually active women to undergo regular pelvic exams and screenings for STIs, as these can help detect PID in its early stages, even before symptoms manifest.
| When to Seek Medical Attention: |
|---|
| If you experience any of the following symptoms, it is important to seek prompt medical attention: |
| – Severe abdominal pain |
| – High fever (above 101°F or 38.3°C) |
| – Fainting or dizziness |
Early detection of PID is crucial for successful treatment and prevention of long-term complications. If you suspect you may have PID or are experiencing any of the symptoms mentioned above, it is important to consult a healthcare professional as soon as possible. Remember, early intervention can make a significant difference in your health and well-being.
Seeking Prompt Medical Attention
When it comes to addressing any health issue, seeking prompt medical attention is crucial. This is especially true when it comes to pelvic inflammatory disease (PID). PID is a serious condition that affects the female reproductive organs and can lead to long-term complications if not treated promptly. In this blog post, we will discuss the importance of seeking immediate medical attention if you suspect you may have PID.
One of the main reasons why seeking prompt medical attention is vital when it comes to PID is the potential for long-term complications. If left untreated, PID can cause permanent damage to the reproductive organs, leading to infertility or an increased risk of ectopic pregnancies. By seeking medical help early on, healthcare professionals can administer appropriate treatment to prevent these complications and preserve your reproductive health.
In addition to preventing long-term complications, seeking immediate medical attention for PID can also help alleviate symptoms and discomfort. PID is often associated with symptoms such as pelvic pain, abnormal vaginal discharge, painful urination, and fever. These symptoms can be distressing and disrupt your daily life. By seeing a healthcare provider promptly, you can receive the necessary treatment and medications to alleviate these symptoms and promote a speedy recovery.
- seeking prompt medical attention for PID is important for preventing the spread of the infection. PID is often caused by bacterial infections, most commonly transmitted through sexual contact. If left untreated, the infection can spread to other parts of the reproductive system and potentially to sexual partners. By seeking medical help early on, you can receive appropriate treatment to not only treat the infection but also prevent its transmission to others.
| Benefits of Seeking Prompt Medical Attention for PID |
|---|
| Prevents long-term complications: Timely treatment can prevent permanent damage to the reproductive organs and future fertility issues. |
| Alleviates symptoms: Prompt medical attention can help alleviate pelvic pain, vaginal discharge, and other discomforting symptoms associated with PID. |
| Prevents spread of infection: Seeking timely treatment prevents the further spread of the bacterial infection causing PID. |
The Impact Of Hygiene On Pid Prevention
In order to prevent Pelvic Inflammatory Disease (PID), it is important to understand the impact of hygiene practices. Good hygiene plays a key role in preventing the spread of bacteria that can lead to PID. By practicing proper hygiene, individuals can significantly reduce their risk of developing this condition.
Regular handwashing is one of the simplest and most effective ways to maintain hygiene and prevent the spread of bacteria. Hands should be washed thoroughly with soap and water before and after using the restroom, before handling food, and after coming into contact with potentially contaminated surfaces. This helps to remove any harmful bacteria that may be present and reduces the risk of introducing it into the reproductive system.
Maintaining cleanliness in the genital area is also important for preventing the development of PID. It is recommended to clean the genital area daily with mild soap and water. Proper wiping techniques after using the restroom should be used, always wiping from front to back to prevent the spread of bacteria from the anus to the vagina. it is important to avoid using harsh irritants, such as douches or scented products, as they can disrupt the natural balance of bacteria in the vagina and increase the risk of infection.
Practicing safe sex is another important aspect of hygiene when it comes to preventing PID. Using barrier methods of contraception, such as condoms, can help reduce the risk of sexually transmitted infections (STIs) that can lead to PID. It is also important to be mindful of sexual partners’ hygiene practices and to have open communication about sexual history and STI status. By taking these precautions, individuals can minimize the risk of contracting infections that may ultimately result in PID.
- SUMMARY TABLE:
| Hygiene Practices | Impact on PID Prevention |
|---|---|
| Regular handwashing | Reduces the spread of bacteria |
| Maintaining cleanliness in the genital area | Prevents bacterial infections |
| Practicing safe sex | Reduces the risk of STIs and subsequent PID |
Preventing Pid After Gynecological Procedures
Gynecological procedures such as hysterectomy, dilation and curettage (D&C), and endometrial biopsy are common medical interventions that women may undergo. While these procedures are performed for various reasons, it is important to recognize the potential risk of developing pelvic inflammatory disease (PID) as a result. PID occurs when bacteria from the vagina or cervix travel into the uterus, fallopian tubes, or ovaries, leading to infection and inflammation. In order to minimize the risk of PID after gynecological procedures, several preventive measures should be followed.
Educating Patients About the Procedure
One of the crucial steps in preventing PID after gynecological procedures is ensuring that patients are well-informed about the intended intervention. Proper patient education should encompass a detailed explanation of the procedure, its purpose, and the potential risks involved. This should include a discussion about the possible development of PID and the symptoms to watch out for post-procedure. By providing patients with comprehensive information, they can be more attentive to any signs of infection or complication, enabling them to seek prompt medical attention.
Utilizing Antibiotic Prophylaxis
In cases where gynecological procedures pose a higher risk of infection, antibiotic prophylaxis is recommended. Antibiotic prophylaxis involves the administration of antibiotics before and after the procedure to prevent infection. This practice helps eliminate any existing bacteria in the reproductive organs and reduces the chances of post-procedure PID development. It is important for healthcare providers to assess the patient’s medical history, previous infections, and any known allergies to prescribe the appropriate antibiotics and dosages.
Maintaining Strict Hygiene Practices
Strict adherence to proper hygiene practices is vital to prevent PID after gynecological procedures. This includes sterilizing medical instruments and equipment, as well as ensuring a clean and sterile environment during the procedure. healthcare providers should follow proper hand hygiene protocols, using hand sanitizers or washing their hands thoroughly before and after the procedure. By maintaining a sterile environment and implementing rigorous hygiene practices, the risk of introducing bacteria into the reproductive organs can be greatly reduced.
Conclusion
Preventing PID after gynecological procedures requires a multi-faceted approach that involves educating patients, utilizing antibiotic prophylaxis, and maintaining strict hygiene practices. By empowering patients with knowledge about the procedure and its potential risks, they can actively participate in their own healthcare and seek immediate medical attention if necessary. Furthermore, the use of antibiotics before and after procedures and the implementation of rigorous hygiene protocols significantly reduce the chances of developing PID. Practicing these preventive measures is crucial to ensure the successful outcome of gynecological procedures and the overall reproductive health of women.
Partner Communication And Mutual Consent
Effective partner communication and mutual consent play a crucial role in promoting healthy and safe sexual practices. In today’s blog post, we will delve into the significance of open communication and consent in maintaining strong and respectful relationships, as well as preventing the transmission of sexually transmitted infections (STIs) and pelvic inflammatory disease (PID).
When engaging in sexual activities, it is essential for partners to be able to openly discuss their desires, boundaries, and concerns. Effective communication fosters trust and understanding, creating a safe space where both partners can freely express their needs and preferences. By openly discussing topics such as sexual history, STI testing, and contraceptive methods, partners can make informed decisions that prioritize their health and well-being.
Mutual consent is another vital aspect of a healthy sexual relationship. Consent should be ongoing and enthusiastic, ensuring that all parties involved are actively and willingly participating. Consent cannot be assumed or pressured; it must be explicitly discussed and obtained before any sexual activity. By practicing mutual consent, individuals can foster an environment of trust, respect, and shared responsibility.
- Open communication and mutual consent can greatly contribute to the prevention of STIs and PID. By openly discussing sexual history and potential risks, partners can make informed decisions about using barrier methods such as condoms or dental dams. effective communication ensures that both partners are aware of the importance of regular STI testing, which can help identify infections early and prevent their spread to others.
- A table illustrating the different types of contraceptives and their effectiveness can serve as a helpful reference for couples when discussing contraceptive options. It can highlight the importance of dual protection – utilizing both barrier methods and hormonal contraceptives – to minimize the risk of unintended pregnancies and STI transmission. By providing accurate and up-to-date information about contraception, individuals can make informed decisions that best suit their needs and preferences.
- effective partner communication and mutual consent are integral to promoting healthy and safe sexual practices. By openly discussing desires, boundaries, and concerns, individuals can establish strong relationships built on trust and understanding. Practicing ongoing and enthusiastic mutual consent ensures that all parties actively participate in sexual activities willingly. By prioritizing open communication and consent, individuals can reduce the risk of STI transmission and PID, creating a safer and more fulfilling sexual experience for both partners.
| Contraceptive Method | Effectiveness |
|---|---|
| Barrier methods (condoms, dental dams) | High when used correctly and consistently |
| Hormonal contraceptives (e.g., birth control pills, implants) | High when used correctly |
| Long-acting reversible contraceptives (e.g., IUDs) | High |
| Sterilization (tubal ligation or vasectomy) | Very high |
The Benefit Of Regular Pelvic Exams
Regular pelvic exams are a crucial aspect of women’s healthcare that offer numerous benefits. These exams are typically performed by a gynecologist or other healthcare provider and involve a careful examination of the reproductive organs, including the uterus, ovaries, fallopian tubes, and cervix. While the frequency may vary depending on a woman’s age, medical history, and risk factors, regular pelvic exams are essential for maintaining overall reproductive health and detecting any potential issues early on.
One of the key benefits of regular pelvic exams is the early detection of various gynecological conditions, including ovarian cysts, uterine fibroids, and pelvic inflammatory disease (PID). These exams can help identify the presence of abnormal growths or infections that may not cause noticeable symptoms initially. Early detection plays a crucial role in successful treatment and management of these conditions, preventing potential complications and improving overall outcomes for the patient.
Furthermore, regular pelvic exams also serve as a vital preventive measure against cervical cancer. During the exam, the healthcare provider may perform a Pap smear, which involves collecting cells from the cervix to screen for any abnormal changes. Cervical cancer, if detected early through regular Pap smears, is highly treatable and has a significantly higher survival rate. Thus, incorporating regular pelvic exams into one’s healthcare routine can significantly reduce the risk of developing cervical cancer and ensure timely intervention if any abnormalities are detected.
- Aside from the diagnostic benefits, regular pelvic exams also provide an opportunity for open communication with healthcare providers. These exams offer a safe and private space for individuals to discuss any concerns or ask questions regarding their sexual and reproductive health. This open dialogue fosters a sense of trust between the patient and their healthcare provider, encouraging a proactive approach to healthcare and facilitating personalized care based on individual needs and circumstances.
- Moreover, regular pelvic exams can contribute to overall mental and emotional well-being by promoting a sense of control and empowerment over one’s health. By actively participating in monitoring and maintaining their reproductive health, individuals can develop a deeper understanding of their bodies and take ownership of their well-being. This proactive approach can alleviate anxiety and uncertainty related to reproductive health concerns and empower individuals to make informed decisions about their healthcare.
| Benefits of Regular Pelvic Exams: |
|---|
| Early detection of gynecological conditions |
| Preventive measure against cervical cancer |
| Opportunity for open communication with healthcare providers |
| Promotes a sense of control and empowerment over one’s health |
regular pelvic exams play a vital role in maintaining and promoting women’s reproductive health. Through early detection, they allow for timely intervention in various gynecological conditions and reduce the risk of developing cervical cancer. Furthermore, these exams facilitate open communication with healthcare providers, fostering trust and ensuring personalized care. The sense of control and empowerment gained from regular pelvic exams contributes to overall mental and emotional well-being. Therefore, prioritizing regular pelvic exams as part of women’s healthcare routine is crucial for proactive management and prevention of potential reproductive health issues.
Education And Awareness: Spreading The Word About Pid
Educating and raising awareness about Pelvic Inflammatory Disease (PID) is crucial in preventing its occurrence and reducing its impact on women’s health. PID is a serious infection of the female reproductive organs, including the uterus, fallopian tubes, and ovaries. It can lead to severe complications, such as infertility, chronic pelvic pain, and ectopic pregnancy. Therefore, spreading information about PID is essential in ensuring early detection, prompt treatment, and prevention of the disease.
One of the key aspects of education and awareness about PID is to emphasize the importance of safe sexual practices. Practicing safe sex by using barrier methods, such as condoms, can significantly reduce the risk of contracting sexually transmitted infections (STIs) that often lead to PID. Educating individuals about the potential consequences of unprotected sex and providing information on available preventive measures are vital in minimizing the prevalence of PID.
another crucial factor in spreading awareness about PID is encouraging partner communication and mutual consent. Open dialogue between partners regarding sexual health and past infections can help identify asymptomatic STIs and prompt early testing and treatment. Promoting a culture of consent and shared responsibility in sexual relationships plays a vital role in preventing the transmission of STIs, including PID.
| Preventing PID after gynecological procedures | The role of contraception in PID prevention | Recognizing and treating STIs |
|---|---|---|
| Providing information on proper post-procedure care and emphasizing the importance of following healthcare provider’s instructions to prevent PID. | Highlighting the various contraceptive methods available, their effectiveness, and the role of contraception in preventing STIs and PID. | Raising awareness about the signs and symptoms of common STIs, as well as the importance of early diagnosis and treatment to prevent the development of PID. |
- The impact of hygiene on PID prevention
- Early detection: signs and symptoms of PID
- Seeking prompt medical attention
Furthermore, promoting good personal hygiene practices is essential in preventing PID. Maintaining proper hygiene during menstruation, such as regular changing of sanitary pads or tampons, and avoiding the use of douches or other harsh feminine hygiene products can help prevent the introduction of bacteria into the reproductive organs.
Recognizing the early signs and symptoms of PID is crucial in seeking timely medical intervention. Common symptoms include abdominal pain, abnormal vaginal discharge, painful urination, irregular menstrual bleeding, and fever. By providing information on these indicators, individuals can be encouraged to seek medical attention promptly, preventing further complications and potential long-term consequences.
creating awareness about PID requires promoting the benefit of regular pelvic exams. Routine pelvic examinations help identify any abnormalities, detect early signs of infection or inflammation, and enable healthcare providers to intervene promptly. By emphasizing the importance of regular check-ups, individuals can understand the significance of preventive healthcare and take steps to prioritize their reproductive health.